¶ TL;DR
- Saves ~$50 Billion Annually: Reduces global clinical trial costs (~$100B/year market) by a baseline of 50%, with up to 95% savings in optimal scenarios.
- 463:1 Return on Investment: A modest annual operational cost of ~$40M generates ~$50B in industry-wide savings, yielding an NPV of ~$249B over 10 years.
- Generates 840,000 Life-Years Annually: The platform is projected to produce a baseline of 840,000 Quality-Adjusted Life Years (QALYs) each year through faster drug access, new therapies, and better prevention.
- Dominant Health Intervention: With an ICER of -$59,501 per QALY, the dFDA is a dominant intervention—it both saves money and improves health.
- $137M+ Daily Cost of Inaction: Each day without the dFDA represents a societal opportunity cost of ~$137M in economic waste and ~2,301 lost QALYs.
¶ Executive Summary
The Challenge: Medical research and development is critically hampered by slow, expensive processes and limited patient access to trials. Current clinical trial paradigms often cost billions and take a decade per new therapy, hindering innovation and delaying access to life-saving treatments.
The dFDA Solution: This analysis outlines the economic and health benefits of transforming the current regulatory framework into a global, decentralized, autonomous FDA (dFDA) platform. Leveraging real-world data and enabling massive, continuous, and highly efficient decentralized clinical trials, this vision is supported by foundational legislation like the "Right to Trial and FDA Upgrade Act", which proposes an "FDA v2 Platform" as a key implementation step.
Transformative Benefits:
- Dramatic Cost Reductions: The dFDA model projects average R&D clinical trial cost savings of 50%, with exceptionally efficient designs (akin to the UK's RECOVERY trial, which achieved up to 80-100x+ cost reduction) potentially achieving up to 95% reduction. This translates to tens of billions of dollars in annual savings from the estimated $100 billion global annual clinical trial expenditure (source 2, see Market Size and Impact).
- Accelerated Innovation & Access: Faster, cheaper trials allow for a vastly increased volume and diversity of tested therapies, including those for rare diseases and unpatentable treatments, significantly speeding up the delivery of new medicines to patients.
- Improved Health Outcomes: The dFDA is projected to generate a baseline of 840,000 Quality-Adjusted Life Years (QALYs) annually. This figure, detailed in a full model in the appendix, is a composite of benefits from faster drug access, enhanced preventative care enabled by real-world data, and new therapies for rare and neglected diseases (see Appendix for full model.
Exceptional Economic Value:
- Return on Investment (ROI): The dFDA platform demonstrates an exceptionally high ROI. Based on core platform operational costs (ROM estimate 40 million USD per year including medium broader initiative costs) against $50 billion in annual R and D savings (50% reduction scenario, Fortune Business Insights, see Market Size and Impact), the NPV analysis yields ROI estimates ranging from 66:1 to 2,577:1 depending on total ecosystem costs (see Full Range ROI Sensitivity Analysis), with a central estimate of approximately 463:1 over 10 years. This high ratio reflects the platform's significant leverage: a relatively modest investment in a global software infrastructure that generates vast savings across the entire pharmaceutical R&D industry.
- Cost-Utility (ICER): The dFDA is a dominant health intervention, meaning it simultaneously saves substantial costs and improves health outcomes. The incremental cost-effectiveness ratio (ICER) is strongly negative (e.g., approximately -$59,501 per QALY gained, ICER, see Appendix A.2.3) for core platform operations plus medium broader initiative costs), far exceeding standard government value thresholds (ICER Reference Case).
- Daily Opportunity Cost of Inaction: Each day the current paradigm is maintained represents a societal opportunity cost of approximately $137 million in forgone economic efficiencies and 2,301 in lost Quality-Adjusted Life Years (QALYs).
Conclusion: The dFDA initiative represents a paradigm shift with the potential for profound societal and economic benefits. Its ability to drastically lower costs, accelerate medical innovation, and improve public health makes a compelling case for its implementation, supported by legislative frameworks such as the "Right to Trial & FDA Upgrade Act."
Below is a conceptual, high-level analysis of the costs, benefits, and return on investment (ROI) for transforming the U.S. Food and Drug Administration's (FDA) current regulatory framework into a "global decentralized, autonomous FDA." This future-state platform would continuously rank treatments using the entirety of clinical and real-world data (RWD), and would enable anyone—potentially over a billion people worldwide—to participate in large-scale, continuous, decentralized clinical trials. This analysis supports the economic rationale for initiatives such as the "Right to Trial and FDA Upgrade Act", which proposes a foundational "FDA v2 Platform" to begin actualizing this vision within the U.S. framework, potentially serving as a model for broader global collaboration.
Because this analysis deals with an innovative and unprecedented transformation, many assumptions must be clearly stated, and the data points are best understood as estimates or ranges. Nonetheless, this exercise provides a structured way to think about potential costs, savings, and impacts on medical progress.
¶ Overview of the Proposed Transformation
¶ Vision
- A global, autonomous regulatory network (not confined to a single government entity) that continuously collects data from real-world use and decentralized clinical trials.
- An open data architecture that aggregates anonymized health data from billions of people, covering foods, drugs, devices, supplements, and other interventions.
- Treatment rankings, continuously updated based on observational and randomized data, personalized by patient characteristics (e.g., genomics, comorbidities).
¶ Key Capabilities
- Massive Decentralized Trials: Patients anywhere can opt in to trials comparing multiple treatments, with automated randomization, data collection (via electronic health records, wearables, apps), and analytics.
- Real-Time Surveillance: Continuous data ingestion about side effects, efficacy, interactions with other drugs/foods, and long-term outcomes.
- Reduced Administrative Overhead: Blockchain or similar decentralized infrastructure for consent management, compensation, and data integrity could replace large swaths of current paperwork, monitoring, and site management costs.
¶ Potential Impact on the Status Quo
- Speed of Trials: Reduced overhead and automated data capture can compress timelines.
- Cost of Trials: Leveraging existing healthcare encounters, telemedicine, and EHR data to drastically cut per-patient costs (modeled on the Oxford RECOVERY trial success).
- Scale & Scope: Potential for testing many more drugs, off-label indications, unpatentable treatments, nutraceuticals, and personalized medicine approaches.
- Innovation Incentives: Lower R&D costs can increase profitability and encourage more entrants/innovation in the life sciences.
¶ Assumptions
¶ Participation and Data Infrastructure
- At least 1 billion people worldwide opt in to share health data in anonymized form.
- Medical records and wearable data are interoperable and standardized sufficiently to be aggregated globally.
- Robust data security and privacy technologies are in place to comply with international regulations (HIPAA, GDPR, etc.).
¶ Cost Reductions
¶ Decentralized trial costs modeled on Oxford RECOVERY
- Decentralized trial costs drop closer to the Oxford RECOVERY model: from an average of $40,000 - $120,000 per patient in traditional Phase III trials (source 2, source 3) to roughly $500 - $1,000 per patient (RECOVERY Trial).
- Regulatory oversight is streamlined through a continuous data audit system, reducing substantial administrative overhead.
¶ Technical Feasibility
- The necessary digital infrastructure (electronic health records, secure data exchange protocols, machine learning analytics, etc.) is assumed to be widely adopted.
- Some advanced technologies (e.g., blockchain, federated learning) achieve maturity to ensure data integrity and patient privacy.
¶ Funding and Governance
- Start-up costs may be shared by governments, philanthropic organizations, and industry.
- Ongoing operational costs are partially offset by reduced labor needs for conventional site-based trials and by subscription or service models from industry sponsors using the platform.
These assumptions set a stage where the platform can indeed function at scale, but this remains a forward-looking scenario.
¶ Costs of Building and Operating the Global Decentralized FDA ROM Estimate
Section Summary
- Upfront core platform build: $37.5–$46 million
- Annual core platform operations: $11–$26.5 million
- Broader initiative (medium scenario): $228 million upfront, $21.3 million annual
- Best case total initiative: ~$4.5M upfront, near $0 annual
- Worst case total initiative: ~$2.2B+ upfront, $271M+ annual
Key Takeaway: The core technology platform is achievable for tens of millions, but full global rollout and integration could require hundreds of millions to billions depending on scope and execution. See detailed breakdowns below.
This section provides a Rough Order of Magnitude (ROM) cost estimate based on the components outlined in the .
¶ Upfront (Capital) Expenditure Initial Build Illustrative 30 Months
-
Core Engineering & Development Effort:
- Basis: ~75 FTEs 2.5 years $200k/FTE/year
- Activities: Detailed design, core platform development (API, storage, mapping/validation, auth), reference frontend, initial plugin interfaces, testing, documentation, initial deployment.
- Estimated ROM: $35 - $40 Million
-
Infrastructure Setup & Initial Cloud Costs:
- Activities: Establishing cloud accounts, VPCs, Kubernetes cluster (EKS) setup, database provisioning (RDS/TimescaleDB), S3 buckets, CI/CD pipeline setup, initial IaC development (Terraform).
- Costs: Includes initial compute/storage during development/testing, potential small upfront reservations.
- Estimated ROM: $1 - $3 Million
-
Software Licenses & Tooling (Initial):
- Examples: Potential costs for monitoring tools (Datadog), security scanners (Snyk), specialized libraries, collaboration tools if not already covered.
- Estimated ROM: $0.5 - $1 Million
-
Compliance, Legal & Security (Initial Setup):
- Activities: Initial HIPAA/GDPR compliance assessment, policy development, security architecture review, legal consultation for data sharing frameworks.
- Estimated ROM: $1 - $2 Million
Total Estimated Upfront Cost (ROM): $37.5 - $46 Million
Note: This ROM estimate focuses only on the Core Platform build effort and associated setup. It represents the foundational first step. The full vision of the "Right to Trial and FDA Upgrade Act" requires significant additional investment in broader initiatives to achieve its goals of global integration, legal harmonization, and massive scale. These crucial, follow-on costs are estimated separately in the Scenario Based ROM Estimates for Broader Initiative Costs section below and include:
- Global EHR/Data Source Integration Effort: Building/buying connectors for thousands of systems worldwide.
- Large-Scale Plugin Development: Funding the ecosystem of data importers, analysis tools, and visualization plugins.
- International Legal/Regulatory Harmonization: Major diplomatic and legal efforts to create a global standard.
- Global Rollout & Adoption: Costs associated with driving adoption and providing training worldwide.
- Massive-Scale Infrastructure: Scaling hardware and cloud resources beyond initial targets to support millions of users as mandated by the Act.
The following sections provide ROM estimates for both the ongoing operational costs of the core platform and for these essential broader initiatives.
¶ Top-Down Analogous Cost Estimation (Market Comparables)
To complement the bottom-up ROM, we can derive a top-down estimate by examining the total investment raised by leading commercial companies developing decentralized clinical trial (DCT) platforms. This market-based view provides a real-world benchmark for the capital required to build, scale, and operate a sophisticated, global-grade platform.
- Medable: A leader in the DCT platform space, has raised a total of $521 million in capital, achieving a valuation of $2.1 billion as of late 2021. This level of funding represents the capital required to develop a comprehensive SaaS platform, establish a global presence across 60+ countries, and achieve significant market penetration.
- Other DCT Platform Companies: Other companies in the space, such as Science 37 (~$40M raised), Thread (up to $50M raised), and uMotif (~$25.5M raised), show that significant traction and platform development can be achieved with investments in the tens of millions.
Analogous ROM Conclusion:
Based on these market comparables, the total investment required to fund a global dFDA platform initiative—from initial build to widespread adoption—can be estimated to be in the range of $50 million to $500 million.
- The lower end (~$50M) aligns with the capital needed to build a robust platform and achieve initial scale, similar to companies like Science 37 or Thread.
- The upper end (~$500M+) reflects the multi-year investment needed to build a market-leading, feature-rich global platform with a vast ecosystem, analogous to the trajectory of Medable.
This top-down estimate corroborates the findings of the bottom-up analysis. While a core, open-source platform can be initiated for tens of millions (as shown in the upfront build ROM), a fully-realized, globally adopted dFDA ecosystem represents a multi-hundred-million-dollar undertaking, consistent with the "Medium Case" and "Worst Case" scenarios for broader initiative costs.
¶ Annual Operational Costs Illustrative at Target Scale of 5M MAU 50TB Ingest Month
-
Cloud Infrastructure Costs (AWS):
- Components: EKS cluster, RDS/TimescaleDB hosting, S3 storage & requests, SQS messaging, API Gateway usage, Data Transfer (egress), CloudWatch logging/monitoring.
- Basis: Highly dependent on actual usage patterns, data retrieval frequency, processing intensity. Assumes optimized resource usage.
- Estimated ROM: $5 - $15 Million / year (Very sensitive to scale and usage patterns)
-
Ongoing Engineering, Maintenance & Operations:
- Team Size: Assume ~20 FTEs (SREs, DevOps, Core Maintainers, Security).
- Basis: 20 FTEs * $200k/FTE/year
- Estimated ROM: $4 - $6 Million / year
-
Software Licenses & Tooling (Ongoing):
- Examples: Monitoring (Datadog/New Relic), Error Tracking (Sentry), Security Tools, potential DB license/support costs at scale.
- Estimated ROM: $0.5 - $1.5 Million / year
-
Compliance & Auditing (Ongoing):
- Activities: Regular security audits (penetration tests, compliance checks), maintaining certifications, legal reviews.
- Estimated ROM: $0.5 - $1 Million / year
-
Support (User & Developer):
- Activities: Tier 1/2 support for platform users and potentially third-party plugin developers.
- Estimated ROM: $1 - $3 Million / year (Scales with user base)
Total Estimated Annual Operations (Platform Only, ROM): $11 - $26.5 Million / year
¶ Marginal Cost Analysis per User
The 5M MAU target is an illustrative milestone used for these initial ROM estimates, not the ultimate goal for the platform, which aims to support hundreds of millions or billions of users. At this initial scale, we can analyze the cost on a per-user basis.
- Average Cost Range Per User (at 5M MAU):
- Based on the total annual operational cost range of $11M - $26.5M, the average cost per user is:
- Marginal Cost Per Additional User:
- As a large-scale software platform, the dFDA system has high fixed costs (infrastructure, core engineering) but very low variable costs. Therefore, the marginal cost of supporting one additional user is expected to be a small fraction of the average cost, likely pennies per year. This cost will decrease further as the platform achieves greater economies of scale, making the system exceptionally efficient at supporting a global user base.
(Note: The underlying cloud infrastructure cost ($5M-$15M/year) is a top-down ROM estimate. A more granular, bottom-up analysis based on projected per-user storage, data transfer, and compute would provide further support for these figures and is a key area for future refinement of this model.)
*Note on Participant Financial Contributions and NIH Cost Discounts (Alignment with "Right to Trial & FDA Upgrade Act"):
This core platform operational cost estimate focuses on the technology infrastructure and does not include the direct financial transactions related to individual trial participation. The "Right to Trial & FDA Upgrade Act" (specifically SEC. 303 and SEC. 304) outlines a model where:
1. Sponsor-Determined Participation Costs: Sponsors itemize the direct costs of a patient's participation in a trial (SEC. 304(a)).
2. NIH-Funded Direct Discount: The NIH Trial Participation Cost Discount Fund directly covers a portion of these patient-borne costs. The specific percentage or amount of this discount is determined by an NIH-managed allocation algorithm aiming to maximize QALYs and other public health benefits (SEC. 303(b, c)). For initial operationalization, while the full algorithm is developed and sufficient data is accrued via the platform, a standardized default discount (e.g., the NIH Fund covering 50% of patient-borne costs) could be applied as a baseline policy. This would allow subsidies to flow quickly, with the mechanism evolving towards the dynamic, data-driven algorithm over time as envisioned in the Act.
3. Patient Net Cost Contribution: The patient is responsible for the remaining net cost after the NIH discount is applied (SEC. 304(b)).
4. Platform Facilitation: The dFDA platform's role, as costed in its operational ROM, includes modules (like the Trial Cost and Discount Module per SEC. 204(c)(3)) to transparently display the itemized costs, the NIH-funded discount, and the final net patient contribution. The platform facilitates the management of these financial components but does not itself disburse the NIH funds or determine the discount amounts.
Large-scale figures sometimes discussed for "participant support" or "subsidies" would primarily reflect the total budget and impact of the NIH Trial Participation Cost Discount Fund, not operational outlays by the dFDA platform for direct compensation (which is not part of this model).
This estimate also excludes costs associated with running the DAO governance structure itself and the cost of developing and maintaining the plugin ecosystem (though some plugin development could be incentivized via platform-specific bounties as per the Act).
¶ Enhanced ROM Estimates and Cost Optimization
Disclaimer: This subsection presents ROM estimates that incorporate the full technical requirements from the "Right to Trial & FDA Upgrade Act" while leveraging cost-saving strategies. The estimates assume successful implementation of open-source development, bounty programs, and AI automation to minimize costs.
Key Cost-Saving Strategies:
- Open-Source Development Model: Leveraging global developer community contributions under permissive licenses (Apache 2.0/MIT).
- Bounty & Prize Programs: Using targeted bounties for specific features, security audits, and integration components.
- AI-Automated Development: Utilizing AI coding assistants and automated testing to reduce development time and costs.
- Modular Architecture: Enabling parallel development of components by different teams/contributors.
- Existing Open-Source Components: Leveraging and contributing back to existing healthcare/blockchain projects.
ROM Estimates by Technical Component:
-
Blockchain Supply-Chain Ledger
- Components: Zero-knowledge proof implementation, DSCSA integration, IoT device integration
- Cost Reduction: Open-source blockchain frameworks, community bounties for core components
- Estimated ROM: 2M USD upfront / 0.5M USD annual maintenance
-
Patient Portal & Treatment Ranking System
- Components: Real-time ranking algorithm, outcome labels, mobile/SMS/IoT interfaces
- Cost Reduction: Open-source frontend frameworks, community-developed plugins
- Estimated ROM: 1.5M USD upfront / 0.3M USD annual maintenance
- Interoperability & API Infrastructure
- Components: FHIR-R5 server, EHR integration adapters, OAuth 2.0 implementation
- Cost Reduction: Existing open-source healthcare APIs, community-contributed adapters
- Estimated ROM: 1M USD upfront / 0.2M USD annual maintenance
- Security & Compliance
- Components: FedRAMP-Moderate compliance, annual pen testing, security monitoring
- Cost Reduction: Bug bounty program, automated security scanning
- Estimated ROM: 0.5M USD upfront / 0.5M USD annual
- AI/ML Capabilities
- Components: Protocol validation, patient-trial matching, safety signal detection
- Cost Reduction: Open-source ML models, transfer learning, community datasets
- Estimated ROM: 1M USD upfront / 0.3M USD annual
- Developer & Community Infrastructure
- Components: Documentation, SDKs, CI/CD pipelines, community support
- Cost Reduction: Automated documentation generation, community moderation
- Estimated ROM: 0.5M USD upfront / 0.2M USD annual maintenance
- Governance & Transparency
- Components: Technical Steering Committee operations, public metrics dashboards
- Cost Reduction: Automated reporting, community governance tools
- Estimated ROM: 0.2M USD upfront / 0.1M USD annual
Total Estimated Development (Upfront): 6.7M USD
Total Estimated Annual Operations: 2.1M USD
¶ Cost Optimization Strategies and Risk Mitigation
Bounty Program Implementation:
- $1M annual budget for security bounties and feature development
- Structured as graduated rewards based on impact and complexity
- Community-voted prioritization of bounty targets
Open-Source Community Building:
- Developer documentation and starter kits ($0.2M initial)
- Hackathons and community events ($0.3M annual)
- Contributor recognition program ($0.1M annual)
AI-Assisted Development:
- AI code generation and review tools ($0.5M initial setup)
- Automated testing and validation pipelines ($0.3M annual)
- Continuous training of domain-specific models ($0.2M annual)
Risk Mitigation:
- 20% contingency buffer on all estimates
- Phased rollout with clear milestones
- Regular third-party security audits
Total Estimated ROM with Optimization:
- Upfront (Year 1): $8.5M (including contingency)
- Annual Operations (Years 2+): $3.0M (including bounties and community programs)
Note: These optimized ROM estimates reflect a strategic approach leveraging open-source, community engagement, and AI to deliver the comprehensive dFDA platform capabilities mandated by the Act in a cost-effective manner. The success of this model hinges on robust community participation and effective management of bounty and prize programs.
¶ Scenario Based ROM Estimates for Broader Initiative Costs
This table presents point estimates for each scenario, with the overall range of possibilities captured by comparing the Best, Medium, and Worst Case columns.
| Component | Best Case (Upfront / Annual) | Medium Case (Upfront / Annual) | Worst Case (Upfront / Annual) | Key Assumptions & Variables Driving Range |
|---|---|---|---|---|
| Global Data Integration | $2M / ~$0 | $125M / $10M | $1.5B / $150M | Success of AI/automation, standards adoption, #systems, vendor cooperation. |
| Bounty & Prize Program (Act SEC. 204(i)) | $1M (Prizes) / ~$0 | $15M (Bounties) / $2M | $50M (Major Bounties) / $10M | Success of organic ecosystem growth vs. need to incentivize critical plugin/tool development via bounties. |
| Legal/Regulatory Harmonization | $1.5M / ~$0 | $60M / $3M | $300M / $30M | Effectiveness of AI legal tools, political will, complexity of global law. |
| Global Rollout & Adoption | ~$0 / ~$0 | $12M / $3M | $125M / $30M | Need for training/support beyond platform status, user interface complexity. |
| DAO Governance Operations | ~$0 / ~$0 | ~$1M / $0.3M | ~$6M / $1M | Automation level, need for audits, grants, core support staff. |
| --- TOTAL --- | ~$4.5M / ~$0 | ~$213M / ~$18.3M | ~$1.98B+ / ~$221M+ | Represents total initiative cost excluding core platform build/ops. |
Interpretation:
Even when pursuing efficient strategies, the potential cost for the full dFDA initiative (beyond the core platform) varies dramatically based on real-world execution challenges. The Medium Case suggests upfront costs in the low hundreds of millions and annual costs in the low tens of millions, while the Worst Case pushes towards multi-billion dollar upfront figures and annual costs in the hundreds of millions, dominated by integration, plugin funding, and legal costs if automation and community efforts fall short.
Revised Summary:
Based on the detailed technical specification, a ROM estimate suggests:
- Initial Core Platform Build (~2.5 years): ~$37.5 - $46 Million
- Annual Core Platform Operations (at ~5M MAU scale): ~$11 - $26.5 Million (These platform operational costs are distinct from the financial flows of patient contributions and the NIH Trial Participation Cost Discount Fund, and also exclude plugin ecosystem costs not covered by platform bounties)
This revised, bottom-up ROM highlights that while the core technology platform build might be achievable within tens of millions, the previously estimated billions likely reflect the total cost of the entire global initiative. This includes massive integration efforts, legal frameworks, global rollout, and the financial ecosystem involving participant contributions and the direct NIH-funded discounts to patient costs, rather than direct platform-disbursed compensation. This conclusion is further supported by the top-down analogous estimate derived from market comparables, which points to a total initiative investment in the range of $50 million to $500 million for a commercial-grade equivalent.
¶ Benefit Analysis Quantifying the Savings
This section quantifies the potential societal benefits of the dFDA platform, focusing primarily on R&D cost savings and health outcome improvements.
¶ Market Size and Impact
The global pharmaceutical and medical device R&D market is vast. Annual global spending on clinical trials alone was estimated to be in the range of USD 60-80 billion in 2024, and projected to exceed USD 100 billion by the early 2030s (Fortune Business Insights, May 2024, Global Market Insights, Feb 2024). A significant portion of this expenditure is addressable by the efficiencies dFDA aims to introduce. If dFDA can capture even a fraction of this market by demonstrating superior efficiency and data quality, its economic impact will be substantial.
For this analysis, we use a conservative baseline estimate of $100 billion per year in global clinical trial spending that is potentially addressable by dFDA through decentralization, automation, and real-world data integration. This figure accounts for future market growth and the expanding scope of trials that could benefit from dFDA methodologies.
- Current Average Costs: Various estimates suggest $1.0 - $2.5 billion to bring a new drug from discovery through FDA approval, spread across ~10 years.
- Clinical Trial Phase Breakdown:
- Phase I: $2 - $5 million/trial (smaller scale).
- Phase II: $10 - $50 million/trial (depending on disease area).
- Phase III: $100 - $500 million/trial (large patient populations).
- Per-Patient Phase III Costs: Often $40,000 - $120,000+ per patient (site fees, overhead, staff, monitoring, data management).
¶ Decentralized Trial Costs Modeled on Oxford RECOVERY
-
Oxford RECOVERY: Achieved ~$500 per patient. Key strategies included:
- Embedding trial protocols within routine hospital care.
- Minimizing overhead by leveraging existing staff/resources and electronic data capture.
- Focused, pragmatic trial designs.
-
Extrapolation to New System:
- A well-integrated global platform could approach $500 - $1,000 per patient in many cases, especially for pragmatic or observational designs.
- Up to ~80-100x+ cost reduction cited for RECOVERY vs. typical Phase III trials is an aspirational benchmark, derived by comparing per-patient costs of ~$500-$1,000 against traditional costs of ~$40,000 - $120,000+.
¶ Overall Savings
-
By Reducing Per-Patient Costs
- If a trial with 5,000 participants costs $500 - $1,000/patient, total cost is $2.5 - $5 million, versus $200 - $600 million under traditional models.
- This magnitude of savings can drastically reduce the total cost of clinical development.
-
Volume of Trials & Speed
- Faster, cheaper trials allow more drug candidates, off-label uses, nutraceuticals, and personalized dosing strategies to be tested.
- Shorter development cycles reduce carrying costs and risk, further increasing ROI for sponsors.
- Crowdsourced funding mechanisms, like those established by the Decentralized Institutes of Health (DIH), can further reduce patient costs and direct resources to high-value research.
-
Regulatory Savings
- A single integrated platform with automated data audits cuts bureaucratic duplication across multiple countries, drastically lowering compliance costs.
-
Accelerated Adoption through Legislative Mandates
- Provisions such as a "Right to Trial," as outlined in the "Right to Trial and FDA Upgrade Act", would significantly accelerate the adoption and utilization of the dFDA platform. By guaranteeing patient access to trials via the platform, data generation, network effects, and the realization of cost savings would be expedited, further enhancing the overall benefits projected in this analysis.
-
Increased Competition Among Sponsors Leading to Lower Submitted Trial Costs
- The transparent nature of the dFDA platform, coupled with mechanisms like NIH discount allocations based on value (QALYs per dollar as described in the "Right to Trial & FDA Upgrade Act"), is expected to create a competitive environment. Sponsors will be incentivized to submit the most efficient trial designs and leanest operational costs to the platform to attract NIH support and patient participation, further driving down the overall R&D expenditure beyond just the technical efficiencies of decentralized trials themselves.
¶ Drug Price Reductions from Global Competition and Importation
U.S.-Specific
- U.S. prescription drug prices are 50–90% higher than in peer countries.
- Allowing importation and global competition could conservatively reduce U.S. drug spending by 20–50% for affected drugs.
- Example Calculation: U.S. annual prescription drug spending is ~$360B. If 50% of the market is affected and prices drop by 25%, annual savings = $360B × 0.5 × 0.25 = $45B.
- References:
- Sarnak, D. O., et al. (2017). Paying for Prescription Drugs Around the World: Why Is the U.S. an Outlier?
- Kesselheim, A. S., et al. (2016). The high cost of prescription drugs in the United States.
Beyond direct importation effects, the fundamental efficiencies introduced by the dFDA platform—drastically reduced R&D costs and accelerated development timelines—are anticipated to further enhance overall market competition for medicines. By lowering the barriers to entry for bringing novel therapies, as well as generics and biosimilars, to market, the dFDA can foster a richer landscape of therapeutic alternatives. A greater number of competing products for similar indications is a well-established economic driver for lower final drug prices, benefiting payors and patients alike. While quantifying this specific effect on end-user drug prices is complex and multifactorial, the structural changes proposed by the dFDA strongly support a trend towards increased affordability through enhanced market competition.
¶ Prevention Savings from Increased Preventive Care
U.S.-Specific
- Chronic diseases account for ~90% of U.S. healthcare spending (~$3.7T/year).
- Preventive care is underfunded (~5% of spend); every $1 spent on prevention saves ~$3.
- Doubling effective preventive spending could yield hundreds of billions in annual savings.
- Example Calculation: If preventive spending increases by $205B and each $1 saves $3, additional savings = $205B × 3 = $615B/year.
- References:
- Trust for America's Health. (2013). A Healthier America: Savings from Prevention.
- CMS National Health Expenditure Data (link)
¶ Economic Value of Earlier Access to Treatments VSL QALY
- Faster approvals and access to effective treatments can save lives and improve quality of life.
- Value of a Statistical Life (VSL): U.S. agencies use ~$10M per life saved (DOT 2021 Guidance).
- QALY Framework: Standard willingness-to-pay is $100,000–$150,000 per QALY gained (ICER).
- Example Calculation: If faster access saves 10,000 QALYs/year, annual benefit = 10,000 × 150,000](#parameterization-overall-dfda-platform-impact) = **\$1.5B**. If 10,000 lives are saved, benefit = 10,000 × [ = $1.5B. If 10,000 lives are saved, benefit = 10,000 × $10M = $100B.
- These benefits are additive to direct cost savings and can be substantial depending on the scale of acceleration.
- References:
- U.S. Department of Transportation. (2021). Guidance on Treatment of the Economic Value of a Statistical Life.
- ICER. Value Assessment Framework.
¶ Gross R and D Savings from dFDA Implementation
- Parameter: Percentage reduction in addressable clinical trial costs due to dFDA.
- Source/Rationale:
- Decentralized Clinical Trials (DCTs), a core component of dFDA, have demonstrated potential for significant cost reductions (20-50% or more) through reduced site management, travel, and streamlined data collection (Rogers et al., 2022; Nature, 2024).
- The UK RECOVERY trial, a prime example of efficient trial design akin to dFDA principles, achieved cost reductions of ~80-98% per patient compared to traditional trials (, citing Manhattan Institute and NCBI).
- Note on R&D Savings Estimates: While specific trials like RECOVERY showcase transformative cost-saving potential (>95%), the average quantifiable cost reduction across the full spectrum of decentralized trials is an area of ongoing research and varies significantly based on trial complexity, therapeutic area, and the extent of decentralization. Rogers et al. (2022) in their systematic review noted that there is currently "insufficient evidence to confirm which methods are most effective in trial recruitment, retention, or overall cost" on a generalized basis. The scenarios below therefore present a range, with the "Transformative" scenario reflecting exceptional, RECOVERY-like outcomes.
- Range Used in Sensitivity Analysis:
- Conservative: 30% (saving $30B annually from a $100B addressable spend)
- Base Case: **50% (saving 50B annually)**](#example-parameterization) from a [ from a $100B addressable spend
- Optimistic: 70% (saving $70B annually) from a $100B addressable spend
- Transformative (RECOVERY Trial-like): 95% (saving $95B annually) from a $100B addressable spend
- Rogers, A., De Paoli, G., Subbarayan, S., Copland, R., Harwood, K., Coyle, J., ... & Mackenzie, I. S. (2022). A systematic review of methods used to conduct decentralised clinical trials. British Journal of Clinical Pharmacology, 88(6), 2843-2862. Available at: https://discovery.dundee.ac.uk/ws/files/72718478/Brit_J_Clinical_Pharma_2022_Rogers_A_systematic_review_of_methods_used_to_conduct_decentralised_clinical_trials.pdf
- "DCTs are developing rapidly. However, there is insufficient evidence to confirm which methods are most effective in trial recruitment, retention, or overall cost."
- Valachis, A., & Lindman, H. (2024). Lessons learned from an unsuccessful decentralized clinical trial in Oncology. npj Digital Medicine, 7(1), 211. Available at: https://www.nature.com/articles/s41746-024-01214-5
- "DCTs are considered cost-saving by reducing the number of onsite patient visits and decreasing the costs related to time for study nurses and clinicians."
- Fortune Business Insights. (May 2024). Clinical Trials Market Size, Share & Industry Analysis. Available at: https://www.fortunebusinessinsights.com/clinical-trials-market-106930
- Provides market sizing, e.g., "The global clinical trials market size was valued at USD 60.94 billion in 2024. The market is projected to grow from USD 64.94 billion in 2025 to USD 104.41 billion by 2032..."
- Global Market Insights. (Feb 2024). Clinical Trials Market – By Phase, By Study Design, By Therapeutic Area, By Service Type – Global Forecast 2024 – 2034. Available at: https://www.gminsights.com/industry-analysis/clinical-trials-market
- Provides market sizing, e.g., "The global clinical trials market accounted for USD 59 billion in 2024. The market is anticipated to grow from USD 62.4 billion in 2025 to USD 98.9 billion in 2034..."
¶ ROI Analysis
The return on investment for the dFDA platform is exceptionally high due to its nature as a leveraged, global software infrastructure. Unlike investments in single drugs or therapies, an investment in the dFDA platform creates systemic efficiencies that benefit the entire R&D ecosystem. The primary economic benefit is the drastic reduction in clinical trial operational costs, which can be redeployed to fund a greater volume and diversity of research.
¶ Methodology
-
Compare Baseline to Future State:
- Baseline: 30–40 new drugs approved annually in the U.S., each costing $1 - $2.5 billion on average for full development and approval. Total R&D spending (industry-wide) is on the order of $90 - $100+ billion per year globally.
- Future State: Potentially hundreds (even thousands) of continuous trials, each at a fraction of the cost. This could double or triple the number of new approvals/indications tested each year and expand to off-patent/unpatented therapies that are currently underexplored.
-
Model Inputs
- Upfront Cost (Core Platform Build): Based on the ROM estimate of ~$37.5 - $46 Million detailed in Upfront (Capital) Expenditure. For ROI calculations, a representative figure (e.g., $40 Million) will be used.
- Annual Operational Cost (Core Platform): Based on the ROM estimate of ~$11 - $26.5 Million / year detailed in Annual Operational Costs.
- Annual Broader Initiative Costs: These can vary significantly, from near zero in optimistic scenarios to tens or hundreds of millions annually. The ROI analysis will consider scenarios, including a "Lean Ecosystem" that combines core platform operational costs with the Medium Case annual broader initiative costs (~$21.3 Million / year) from Scenario-Based ROM Estimates for Broader Initiative Costs.
(Note: The ROI analysis will primarily focus on these ROM-derived costs. Previous high-level conceptual estimates for a fully scaled, long-term global dFDA vision, which were significantly larger, are superseded by these more granular figures from the 'Costs of Building and Operating the Global Decentralized FDA ROM Estimate' section for the purpose of this ROI calculation.) - Cost Reduction: Up to 80× in the biggest, most efficient scenarios; conservative average ~50%–80% reduction in trial costs.
- Increased Throughput: 2×–5× more trials and potentially many more candidates tested in parallel.
- Faster to Market: Potentially 1–3 years shaved off a typical 7–10 year development cycle, yielding earlier revenue generation and extended effective patent life for sponsors.
¶ Simplified ROI Scenario
Initial Note on Operational Costs in this ROI Scenario:
The following ROI calculation primarily uses cost figures derived from the detailed ROM estimates in Costs of Building and Operating the Global Decentralized FDA (ROM Estimate). This includes the core platform build and operational costs, as well as scenarios for broader initiative costs. This approach provides a more grounded basis for the ROI than previous high-level conceptual figures for a fully scaled global ecosystem.
- Industry R&D Spend (Baseline): $100 billion/year globally (approx.).
- Potential Savings: 50% reduction implies $50 billion/year saved if the entire industry migrated.
- Platform Cost Scenarios (Derived from ROM Estimates):
- Upfront Cost (Core Platform Build): ~$40 Million (representative figure from Upfront (Capital) Expenditure).
- Annual Operational Cost Scenarios:
- Scenario 1: Core Platform Only: ~$11 - $26.5 Million / year (from Annual Operational Costs). Let's use a midpoint of ~$19 Million/year for calculation.
- Scenario 2: Lean Ecosystem (Core Platform + Medium Broader Initiatives):
- Core Platform Ops (midpoint from Annual Operational Costs): ~$19 Million/year
- Medium Broader Initiative Annual Costs (from Scenario-Based ROM Estimates): ~$21 Million/year
- Total Lean Ecosystem Annual Cost: ~$19M + ~$21M = ~$40 Million/year (or $0.04 Billion/year). This aligns with the cost basis for the ROI cited in the Executive Summary.
- (Other scenarios, such as including "Worst Case" broader initiative costs from Scenario-Based ROM Estimates, could be considered for sensitivity analysis but would significantly increase annual costs.)
- Net Annual Savings (assuming full adoption and 50% R and D cost reduction): $50 Billion/year.
From a purely financial perspective, if the industry can move to such a platform and achieve these savings:
Let's calculate ROI based on the Lean Ecosystem scenario:
- Upfront Cost (Core Platform Build from Upfront (Capital) Expenditure): $40 Million. Amortized over 5 years: $8 Million/year.
- Annual Operational Cost (Lean Ecosystem - Core Platform Ops from Annual Operational Costs + Medium Broader Initiatives from Scenario-Based ROM Estimates): ~$40 Million/year.
- Total Annualized Cost: $8M (amortized upfront) + $40M (annual ops) = $48 Million/year (or $0.048 Billion/year).
This simplified calculation, based on a basic amortization of upfront costs, yields an exceptionally high ROI. However, a more rigorous Net Present Value (NPV) analysis, which properly discounts future costs and savings, is detailed in Calculation Framework. The NPV analysis provides the final estimated ROI of approximately 463:1, which is the figure cited throughout this document.
¶ Full Range ROI Sensitivity Analysis
To provide a comprehensive view, we can calculate the ROI across the full spectrum of cost possibilities by combining the Core Platform costs with the Broader Initiative scenarios from Costs of Building and Operating the Global Decentralized FDA.
Assumptions for Full Range ROI Calculation:
- Net Annual Savings: $50 Billion/year (from 50% R&D cost reduction).
- Amortization Period for Upfront Costs: 5 years.
¶ 1. Lowest Total Cost Scenario (Best Case Core Platform + Best Case Broader Initiatives)
- Upfront Costs:
- Core Platform Build (Low end from Upfront (Capital) Expenditure): ~$37.5 Million
- Broader Initiatives (Best Case Upfront from Scenario-Based ROM Estimates): ~$4.5 Million
- Total Lowest Upfront Cost: $37.5M + $4.5M = $42 Million
- Amortized over 5 years: $42M / 5 = $8.4 Million/year
- Annual Operational Costs:
- Core Platform Operations (Low end from Annual Operational Costs): ~$11 Million/year
- Broader Initiatives (Best Case Annual from Scenario-Based ROM Estimates): ~$0 Million/year
- Total Lowest Annual Operational Cost: $11 Million/year
- Total Lowest Annualized Cost: $8.4M (amortized upfront) + $11M (annual ops) = $19.4 Million/year
- ROI (Lowest Cost Scenario): $50 Billion / $0.0194 Billion ≈ 2577:1
¶ 2. Highest Total Cost Scenario (Worst Case Core Platform + Worst Case Broader Initiatives)
- Upfront Costs:
- Core Platform Build (High end from Upfront (Capital) Expenditure): ~$46 Million
- Broader Initiatives (Worst Case Upfront from Scenario-Based ROM Estimates): ~$2.231 Billion
- Total Highest Upfront Cost: $46M + $2.231B = ~$2.277 Billion
- Amortized over 5 years: $2.277B / 5 = ~$455.4 Million/year
- Annual Operational Costs:
- Core Platform Operations (High end from Annual Operational Costs): ~$26.5 Million/year
- Broader Initiatives (Worst Case Annual from Scenario-Based ROM Estimates): ~$271 Million/year
- Total Highest Annual Operational Cost: $26.5M + $271M = ~$297.5 Million/year
- Total Highest Annualized Cost: $455.4M (amortized upfront) + $297.5M (annual ops) = ~$752.9 Million/year
- ROI (Highest Cost Scenario): $50 Billion / $0.7529 Billion ≈ 66:1
This full range sensitivity analysis demonstrates that the ROI for the dFDA initiative remains exceptionally positive. Even at the highest conceivable costs derived from the 'Costs of Building and Operating the Global Decentralized FDA ROM Estimate' section, the financial return is substantial.
¶ Broader Impacts on Medical Progress
-
Acceleration of Approvals
- With continuous, real-time data, new drugs, devices, and off-label uses could gain near-immediate or conditional approvals once efficacy thresholds are met.
- Diseases lacking major commercial interest (rare diseases, unpatentable treatments) benefit from much lower trial costs and simpler recruitment.
-
Personalized Medicine
- Aggregating genomic, lifestyle, and medical data at large scale would refine "one-size-fits-all" treatments into personalized regimens.
- Feedback loops allow patients and clinicians to see near-real-time outcome data for individuals with similar profiles.
-
Off-Label & Nutritional Research
- Many nutraceuticals and off-patent medications remain under-tested. Lower cost trials create economic incentives to rigorously evaluate them.
- Could lead to significant improvements in preventive and integrative healthcare.
-
Public Health Insights
- Constant real-world data ingestion helps identify population-level signals for drug safety, environmental exposures, and dietary patterns.
- Better evidence-based guidelines on how foods, supplements, or lifestyle interventions interact with prescribed medications.
-
Innovation & Competition
- Lower barriers to entry for biotech start-ups, universities, and non-profits to test new ideas.
- Potential for new revenue streams (e.g., analytics, licensing validated trial frameworks, etc.), leading to reinvestment in R&D.
-
Healthcare Equity
- Decentralized trials allow broader participation across geographies and socioeconomic groups, improving diversity of data and reducing bias.
- Potentially democratizes access to experimental or cutting-edge treatments.
¶ Data Sources and Methodological Notes
-
Cost of Current Drug Development:
- Tufts Center for the Study of Drug Development often cited for $1.0 - $2.6 billion/drug.
- Journal articles and industry reports (IQVIA, Deloitte) also highlight $2+ billion figures.
- Oxford RECOVERY trial press releases and scientific papers indicating $500 - $1,000/patient cost.
-
ROI Calculation Method:
- Simplified approach comparing aggregated R&D spending to potential savings.
- Does not account for intangible factors (opportunity costs, IP complexities, time-value of money) beyond a basic Net Present Value (NPV) perspective.
-
Scale & Adoption Rates:
- The largest uncertainties revolve around uptake speed, regulatory harmonization, and participant willingness.
- Projections assume widespread adoption by major pharmaceutical companies and global health authorities.
-
Secondary Benefits:
- Quality-of-life improvements, lower healthcare costs from faster drug innovation, and potentially fewer adverse events from earlier detection.
- These are positive externalities that can significantly enlarge real ROI from a societal perspective.
¶ Conclusion
Transforming the FDA's centralized regulatory approach into a global, decentralized autonomous model holds the promise of dramatically reducing clinical trial costs (potentially by a factor of up to 80× in some scenarios), accelerating the pace of approvals, and broadening the scope of what treatments get tested. While the full global initiative could involve larger-scale investment over time, the foundational upfront investment for the core technology platform is estimated to be on the order of ~$37.5 - $46 Million, plus ongoing operational costs. Analogous top-down estimates based on market comparables for leading decentralized trial platforms suggest a total initiative investment in the range of $50 million to $500 million to achieve global scale and adoption. However, given that the pharmaceutical industry collectively spends around $100 billion per year on R and D and that a large share of those expenses go to clinical trials, even a 50% reduction in trial costs—combined with faster product launches—would yield enormous net savings and an ROI estimated at approximately 463:1 (with a full range of 66:1 to 2,577:1) once adopted at scale.
Beyond the direct economic benefits, the secondary and tertiary effects on medical progress could be transformative. More drugs, nutraceuticals, and personalized therapies could be tested and refined rapidly; real-time data would continuously update treatment rankings; and off-label or unpatentable treatments—often neglected today—could receive the same rigorous evaluation as blockbuster drugs. If combined with robust privacy controls and global regulatory collaboration, such a platform could usher in a new era of evidence-based, personalized healthcare that benefits patients around the world, drives innovation, and lowers long-term healthcare costs.
¶ Disclaimer
All figures in this document are estimates based on publicly available information, industry benchmarks, and simplifying assumptions. Real-world costs, savings, and ROI will vary greatly depending on the scope of implementation, the speed of adoption, regulatory cooperation, and numerous other factors. Nonetheless, this high-level exercise illustrates the substantial potential gains from a global, decentralized, continuously learning clinical trial and regulatory ecosystem.
¶ Appendix Calculation Frameworks and Detailed Analysis
This appendix provides the detailed models and data used in the cost-benefit analysis.
¶ Calculation Framework
Below is an illustrative framework with more formal equations and a simplified but "rigorous" model to analyze the cost–benefit dynamics and ROI of upgrading the FDA (and analogous global regulators) into a decentralized, continuously learning platform. Many real-world complexities (e.g., drug-specific risk profiles, variable regulatory timelines across countries) would require further refinement, but these equations give a starting point for a more quantitative analysis.
¶ Definitions and Parameters
We define the following parameters to capture costs, savings, timelines, and scaling/adoption:
-
Initial (Upfront) Costs
- : Core platform development (software, AI, UI/UX).
- : Blockchain or other distributed-ledger infrastructure.
- : Integration with EHRs, wearables, privacy/security frameworks.
- : Harmonizing global regulations and legal frameworks.
-
Annual Operating Costs (in year ):
- : Ongoing software maintenance, hosting, cybersecurity.
- : Machine learning, data processing, and analytics costs.
- : Lean administrative overhead, compliance checks, auditing.
- : Compensation or incentives for trial participation.
-
Trial Costs Under Traditional vs. Decentralized Models
- Let be the number of patients in a given trial.
- Traditional cost per patient: .
- Decentralized cost per patient: , where .
Therefore, the total cost for a single trial of size is:
The per-trial savings for patients is then:
-
Industry-Wide R&D Spend & Adoption
- Let be the annual global R&D expenditure on clinical trials (baseline).
- Let be the fraction of R&D cost that can be saved when trials shift to the decentralized model (this encompasses both per-patient cost savings and administrative/overhead reductions).
- Let be the fraction of industry adoption at year . Early on, may be low; over time, it might approach 1 if the platform becomes standard worldwide.
Thus, the annual cost savings in year from using the decentralized model is approximated by:
(This expression assumes full feasibility for all relevant trials and that the fraction is the average cost reduction across all trials.)
-
Discount Rate & Net Present Value
- Let be the annual discount rate (e.g., 5–10% for cost-of-capital or social discounting).
- A future cost (or saving) in year is discounted by .
¶ NPV of Costs
We sum the upfront cost and the net present value (NPV) of ongoing operational costs from to :
¶ NPV of Savings
Using our adoption model and fraction of R&D spend that is saved, the annual savings is . Over years, the total NPV of these savings is:
Note: If the adoption curve grows over time, you might model it with an S-shaped or logistic function. For instance:
where is the steepness of adoption and is the midpoint.
¶ ROI
We define ROI as the ratio of the NPV of total savings to the NPV of total costs:
Alternatively, one might define a net ROI (or net benefit) as:
If , the program yields a positive return in present-value terms.
¶ Example Parameterization
For a concrete (though simplified) scenario, assume:
-
Upfront Costs ():
(This represents an estimated cost for initial core platform build (see Upfront (Capital) Expenditure), foundational broader initiative setup, and early legal/regulatory framework alignment (see medium case upfront costs in Scenario-Based ROM Estimates), consistent with multi-year funding such as in the "Right to Trial and FDA Upgrade Act" for the FDA v2 platform. This combined figure is distinct from the core platform build ROM alone and serves as an illustrative figure for this NPV example that is lower than the previous $3B placeholder.)
-
Annual Operating Costs ():
(This figure is also explicitly derived from the ROM estimates. It represents the sum of the midpoint of the Annual Core Platform Operations from Annual Operational Costs (~$18.75M) and the Medium Case annual costs for Broader Initiatives from Scenario-Based ROM Estimates (~$21.3M). This excludes large-scale, direct participant compensation programs which would be funded separately, as discussed in Annual Operational Costs.)
-
Annual Global R&D Spend ():
-
Fraction of R&D Cost Saved ():
(This is conservative relative to some references suggesting up to 80× savings. It's important to note that these projected R&D savings are achieved not only through the inherent technical and operational efficiencies of decentralized, platform-based trials—e.g., reduced site management, automated data capture—but also through the anticipated competitive pressures the transparent dFDA platform will place on sponsors to optimize trial designs and submit lean, competitive operational cost estimates. See Gross R and D Savings.)*
-
Adoption Curve ():
- Suppose a ramp from 0% adoption at to 100% by . One simple linear approach is:
and for .
- Suppose a ramp from 0% adoption at to 100% by . One simple linear approach is:
-
Discount Rate ():
-
Time Horizon ():
¶ NPV of Costs
- Upfront: .
- Each year: .
Hence,
A standard annuity formula:
Therefore,
So,
¶ NPV of Savings
For to 5, . For to 10, .
- Years 1–5:
- Years 6–10:
Hence,
Let's approximate numerically:
-
For to 5:
- : . Discount factor: . Contribution: .
- : . Discount factor: . Contribution: .
- : . Factor: . Contribution: .
- : . Factor: . Contribution: .
- : . Factor: . Contribution: .
Summing these: .
-
For to 10, . Each year's discount factor:
- : . Contribution: .
- : . Contribution: .
- : . Contribution: .
- : . Contribution: .
- : . Contribution: .
Summing these: .
Thus,
¶ Final ROI and Net Benefit
In this rough example, even partial adoption in the early years delivers large returns. If or were higher, or if the discount rate were lower, the ROI would increase further. This ROI is based on a cost model that is now explicitly derived from the detailed component estimates in the 'Costs of Building and Operating the Global Decentralized FDA ROM Estimate' section, providing a more transparent and verifiable result.
¶ Other Extensions and Considerations
-
Time-to-Market Acceleration
One can add a parameter for the number of years of early market entry. Earlier entry can yield extra revenue or extend effective patent life. A simplified approach might add a term for the "additional value" of each year gained:where is the annual net cash flow gained from earlier commercialization. This can be factored into .
-
Value of Testing More Candidates
Reductions in per-trial costs might double or triple the number of drug candidates tested each year, including off-label indications, nutraceuticals, and personalized therapies. One could introduce a function:where is the baseline number of trials (or new drug approvals) per year, and reflects the increased throughput. The incremental societal or commercial value of these additional approvals can be added to the savings side of the equation.
-
Quality-Adjusted Life Years (QALYs)
For a more health-economic model, incorporate a health outcomes dimension, e.g., QALYs gained from earlier availability of better therapies, or from broader real-world evidence that improves prescribing practices. This would create a cost–utility analysis with:where is the willingness-to-pay per QALY.
-
Risk & Uncertainty
- Real-world constraints (regulatory pushback, privacy laws) might reduce .
- Slower adoption or partial global integration might reduce .
- Incremental infrastructure costs might be higher if existing EHR systems are fragmented.
Even so, the core takeaway remains: If the platform is widely adopted and per-patient trial costs drop substantially, the net benefits likely dwarf the initial investments.
¶ Cost Utility ICER QALY and Sensitivity Analysis
¶ Introduction Why QALY and ICER
To meet the standards of government and health technology assessment (HTA) bodies such as ICER, we present a cost-utility analysis using the incremental cost-effectiveness ratio (ICER) and quality-adjusted life years (QALYs). This approach is the US and global standard for evaluating the value of health interventions (ICER).
-
QALY: One year of life in perfect health. Gains are calculated as:
Where / = quality of life (0-1) before/after, / = years of life before/after.
-
ICER: The cost per QALY gained:
If an intervention saves money (negative incremental cost) and improves health (positive QALY gain), the ICER will be negative, indicating a dominant (cost-saving) intervention.
-
US Willingness-to-Pay Threshold: Typically $100,000–$150,000 per QALY for interventions that add costs (ICER Reference Case). Dominant interventions are favorable regardless of this threshold.
-
Sources for Context:
- "The quality-adjusted life year (QALY) is the academic standard for measuring how well all different kinds of medical treatments lengthen and/or improve patients' lives..." (ICER)
- "ICER's health benefit price benchmark (HBPB) will continue to be reported using the standard range from $100,000 to $150,000 per QALY..." (ICER Reference Case)
¶ Parameterization Overall dFDA Platform Impact
The dFDA platform's primary economic impact comes from significantly reducing R&D costs. Its health impact, measured in Quality-Adjusted Life Years (QALYs), stems from three main pillars: accelerating drug development, enabling better prevention through real-world evidence, and facilitating research for previously untreatable conditions.
A. Net Incremental Cost of dFDA Platform (Annual):
-
Calculated as:
(Platform Operational Costs) - (Gross R and D Savings from dFDA) -
Baseline Assumptions for R&D Savings (same as before):
- Global Clinical Trial Spending Addressable by dFDA: $100 Billion / year.
- R&D Trial Cost Reduction due to dFDA (Baseline): 50%. (Leads to $50B Gross R and D Savings). It's important to note that these projected R&D savings are achieved not only through the inherent technical and operational efficiencies of decentralized, platform-based trials—e.g., reduced site management, automated data capture—but also through the anticipated competitive pressures the transparent dFDA platform will place on sponsors to optimize trial designs and submit lean, competitive operational cost estimates.
-
Aggregate Annual QALYs Gained (ΔQALYs_total): The number of QALYs generated annually by the dFDA platform is a composite metric derived from a detailed model in the appendix. The model provides a range of estimates based on the successful realization of the platform's potential.
- Conservative Scenario: 190,000 QALYs/year
- Base Case Scenario: 840,000 QALYs/year
- Optimistic/Transformative Scenario: 3,650,000 QALYs/year
For a complete breakdown of the assumptions, data sources (including NBER working papers by Glied & Lleras-Muney and Philipson et al.), and calculations behind these figures, please see the Appendix: Detailed QALY Calculation Model.
- Platform Operational Cost Scenarios: The sensitivity analysis below considers various scopes for the platform's operational costs, derived from the Costs of Building and Operating the Global Decentralized FDA ROM Estimate section.
- Core Platform Ops (Midpoint): $0.01875B ($18.75M) / year
- Core Platform + Medium Broader Initiative: $0.04B ($40M) / year
- Illustrative Total Ecosystem (Low-Medium): $0.5B ($500M) / year
- Illustrative Total Ecosystem (High): $5B / year
¶ Sensitivity Analysis Overall dFDA Platform Cost-Effectiveness
This table analyzes the ICER for the dFDA platform by varying key assumptions. Global Clinical Trial Spending Addressable by dFDA is assumed at $100B/year (leading to $50B gross savings in the 50% reduction scenario) unless otherwise specified.
| Scenario | R&D Trial Cost Reduction | Platform Op. Cost (Annual) | Net Incremental Cost (Annual) | Aggregate QALYs Gained (Annual) | ICER (Cost per QALY Gained) | Classification | Source/Note |
|---|---|---|---|---|---|---|---|
| Base Case: Core Platform Ops Only | 50% ($50B Savings) | $0.01875B ($18.75M) | -$49.981B | 840,000 | -$59,501 | Dominant | Ops cost from the 'Annual Operational Costs' ROM midpoint. QALYs from new base model. |
| Core Platform + Medium Broader Initiative | 50% ($50B Savings) | $0.04005B ($40.05M) | -$49.96B | 840,000 | -$59,476 | Dominant | Ops from 'Annual Operational Costs' + 'Scenario Based ROM Estimates for Broader Initiative Costs' (Medium), aligns with ROI calc. |
| Total Ecosystem (Low-Medium Cost) | 50% ($50B Savings) | $0.5B ($500M) | -$49.5B | 840,000 | -$58,929 | Dominant | Illustrative total ecosystem cost. |
| Total Ecosystem (High Cost, e.g. w/ Part. Comp.) | 50% ($50B Savings) | $5B | -$45B | 840,000 | -$53,571 | Dominant | Illustrative high total ecosystem cost (as prior base). |
| Conservative R&D Savings & QALYs | 30% ($30B Savings) | $0.5B ($500M) | -$29.5B | 190,000 | -$155,263 | Dominant | Using Low-Med Ecosystem Cost & Conservative QALY model. |
| Optimistic R&D Savings & QALYs | 70% ($70B Savings) | $0.5B ($500M) | -$69.5B | 3,650,000 | -$19,041 | Dominant | Using Low-Med Ecosystem Cost & Optimistic QALY model. |
| Transformative R&D Savings (RECOVERY Trial-like) | 95% ($95B Savings) | $0.5B ($500M) | -$94.5B | 3,650,000 | -$25,890 | Dominant | Using Low-Med Ecosystem Cost & Optimistic QALY model. |
| Platform Breaks Even (R&D Savings = Ops Cost) | e.g., 0.5% ($0.5B Savings) | $0.5B ($500M) | $0 | 840,000 | $0 | Dominant (Cost-Neutral, Health Gaining) | Using Low-Med Ecosystem Cost & Base QALYs. |
Note: Negative ICER values indicate that the dFDA platform is cost-saving while also improving health outcomes. "Platform Op. Cost" here refers to different scopes: "Core Platform Ops" is per the 'Annual Operational Costs' ROM. Higher figures labeled "Total Ecosystem" are illustrative and aim to include broader initiative costs and/or large-scale participant compensation.
¶ Discussion: Policy Implications
The analysis robustly demonstrates that the dFDA platform is not merely cost-effective but is overwhelmingly a dominant (cost-saving) intervention across a wide range of plausible scenarios, especially when considering the core platform's technical operational costs.
- Massive Cost Savings & Extremely Favorable Core ICER: The core dFDA platform (with operational costs of ~$19M-$40M/year as per the 'Costs of Building and Operating the Global Decentralized FDA ROM Estimate' ROM) generates tens of billions in net annual R and D savings. This results in extremely negative ICERs (e.g., ~-$59,501 per QALY), indicating exceptional value.
- Total Ecosystem Considerations: Even when accounting for significantly broader ecosystem costs (e.g., hundreds of millions or even billions annually for extensive global rollout, governance, plugin development, and/or large-scale participant compensation), the dFDA initiative remains dominant and highly cost-saving, with strongly negative ICERs (e.g., -$19,041 to -$155,263 per QALY in various scenarios).
Summary: The dFDA initiative is projected to be a dominant healthcare transformation. The core technology platform itself is exceptionally efficient (annual operational costs ~$19M-$40M per the 'Costs of Building and Operating the Global Decentralized FDA ROM Estimate' ROM), leading to ICERs around -$59,476 per QALY. Even when considering broader illustrative total ecosystem costs (potentially $0.5B to $5B+ annually to include extensive global operations, participant compensation etc.), the initiative yields substantial net monetary savings (e.g., -$29.5B to -$94.5B annually in various scenarios) while simultaneously generating hundreds of thousands to millions of QALYs each year. The actual cost per QALY gained remains strongly negative across all these scopes, making it an exceptionally high-value proposition.
(Optional: A note could be added here that specific programs built upon the dFDA platform, if they incur additional marginal costs, would then be evaluated for their own cost-effectiveness. However, they would benefit from the already cost-saving nature of the underlying dFDA infrastructure.)
¶ Appendix: Detailed QALY Calculation Model
This model provides a transparent basis for the aggregate annual Quality-Adjusted Life Years (QALYs) generated by the dFDA platform. The total QALY gain is the sum of three distinct benefit streams, each presented with a conservative, base, and optimistic estimate.
¶ A. Accelerating Development of Existing Pipeline Drugs
This stream quantifies the health gains from bringing effective treatments to patients faster. The dFDA platform is expected to shorten development and approval timelines significantly.
- Rationale: a one-year delay in the diffusion of new cancer therapies alone resulted in a loss of 84,000 life-years. By reducing trial times, the dFDA can recapture this value across the entire pharmaceutical pipeline.
- Assumptions:
- Conservative: dFDA achieves a modest acceleration, equivalent to the gains seen in the cancer study.
- Base: A 2-year average acceleration across a broader range of therapies, including but not limited to oncology.
- Optimistic: A more profound acceleration (3+ years) combined with an increased number of successful drugs due to lower trial costs.
- Annual QALY Estimates:
- Conservative: 100,000 QALYs
- Base: 200,000 QALYs
- Optimistic: 400,000 QALYs
¶ B. Improving Preventative Care via Real-World Evidence
This stream captures the value of using the dFDA's continuous real-world data to optimize and personalize preventative medicine, which is currently underutilized.
- Rationale: Research demonstrates that existing cancer screenings have already saved millions of life-years, with much potential still untapped at full adherence. The dFDA platform can identify at-risk populations and measure the real-world effectiveness of preventative interventions (e.g., statins, diabetes screening, lifestyle changes) at a massive scale.
- Assumptions:
- Conservative: The platform leads to modest improvements in adherence and targeting for a few key preventative measures.
- Base: The platform drives significant uptake and better targeting of established preventative care across multiple chronic diseases.
- Optimistic: The platform uncovers new, highly effective preventative strategies and enables their rapid, widespread adoption.
- Annual QALY Estimates:
- Conservative: 50,000 QALYs
- Base: 140,000 QALYs
- Optimistic: 250,000 QALYs
¶ C. Enabling Research for Previously Untreatable/Neglected Diseases
This stream reflects the transformative potential of the dFDA to create viable research pathways for conditions that are currently ignored due to high trial costs and small patient populations, such as rare diseases.
- Rationale: Over 7,000 rare diseases affect 30 million Americans, yet most lack an FDA-approved treatment. The dFDA's radically lower per-patient trial cost makes R&D in this area economically feasible for the first time. A single successful new therapy for a rare disease affecting just 20,000 people could generate over 50,000 QALYs.
- Assumptions:
- Conservative: The platform enables at least one successful new treatment for a smaller rare disease population each year.
- Base: The platform facilitates several new treatments annually or one major breakthrough for a more common rare disease.
- Optimistic: The low-cost model spurs a wave of innovation, leading to dozens of new therapies for rare diseases and other neglected research areas.
- Annual QALY Estimates:
- Conservative: 40,000 QALYs
- Base: 500,000 QALYs
- Optimistic: 3,000,000 QALYs
¶ Summary of Total Annual QALY Gains
| Scenario | (A) Accelerated Development | (B) Improved Prevention | (C) New Research | Total Annual QALYs |
|---|---|---|---|---|
| Conservative | 100,000 | 50,000 | 40,000 | 190,000 |
| Base Case | 200,000 | 140,000 | 500,000 | 840,000 |
| Optimistic | 400,000 | 250,000 | 3,000,000 | 3,650,000 |
¶ DCT Platform Funding (Analogous Cost Basis)
-
$521M raised by Medable
"Decentralized Clinical Trials (DCT) leader Medable, today announced a $304M Series D funding round today – the company's largest and fourth funding round in 18 months, bringing total capital raised to $521M – and valuation to $2B+."
— HIT Consultant, Oct 2021 -
$50M raised by Thread
"Thread, which also specializes in decentralized clinical research technology, revealed last week that it had raised strategic capital commitments of up to $50 million from investors Water Street Healthcare Partners and JLL Partners."
— MobiHealthNews, Aug 2020 -
$40M raised by Science 37
"Another $40 million raise was announced yesterday by decentralized clinical trial startup Science 37."
— MobiHealthNews, Aug 2020 -
$25.5M raised by uMotif
"uMotif today announced a new investment of $25.5m from a fund managed by Athyrium Capital Management, LP"
— Pharma Almanac, Apr 2022
¶ Sources
- "The quality-adjusted life year (QALY) is the academic standard for measuring how well all different kinds of medical treatments lengthen and/or improve patients' lives, and therefore the metric has served as a fundamental component of cost-effectiveness analyses in the US and around the world for more than 30 years." (ICER)
- "ICER's health benefit price benchmark (HBPB) will continue to be reported using the standard range from $100,000 to $150,000 per QALY and per evLYG." (ICER Reference Case)
- "Each year of delayed access to curative therapy for hepatitis C costs 0.2–1.1 QALYs per patient." (Pho et al., 2015)
- "Syphilis causes substantial health losses in adults and children... The average number of discounted lifetime QALYs lost per infection as 0.09." (Lee et al., 2022)
- "Statin treatment provides a gain of 0.20 QALYs in men aged 60 years." (BMJ)
¶ Daily Opportunity Cost of Inaction
This section quantifies the daily societal cost of maintaining the status quo, framed as the opportunity cost of not implementing the dFDA platform. By translating the annualized benefits identified in this analysis into a daily metric, we can better appreciate the urgency of the proposed transformation. The "cost of inaction" is the value of the health gains (QALYs) and financial savings (R&D efficiencies) that are forgone each day the dFDA system is not operational.
¶ Base Case: Daily Lost QALYs and Financial Savings
The calculations below are based on the central ("base case") estimates established in the preceding sections of this analysis.
-
Daily QALYs Lost:
- The analysis (Appendix: Detailed QALY Calculation Model) projects a baseline of 840,000 Quality-Adjusted Life Years (QALYs) gained per year from the dFDA's impact.
- The daily opportunity cost in lost health is therefore:
-
Daily Financial Value Lost:
- The analysis (Gross R and D Savings from dFDA Implementation) projects gross R&D savings of 50 billion per year](#gross-r-and-d-savings-from-dfda-implementation)** by reducing the costs of the [** by reducing the costs of the $100 billion global clinical trial market by 50%. This represents value that is currently being spent inefficiently.
- The daily financial loss from this inefficiency is:
¶ Sensitivity Analysis of Daily Opportunity Costs
The daily costs of inaction are highly sensitive to the underlying assumptions about R&D cost reduction and QALY gains. The following table explores this uncertainty by showing the daily opportunity cost across a range of scenarios, from conservative to transformative, based on the QALY Calculation Model.
| Scenario | R&D Trial Cost Reduction | Annual Gross Savings | Annual QALYs Gained | Daily Money Lost (Approx.) | Daily QALYs Lost (Approx.) | Note |
|---|---|---|---|---|---|---|
| Conservative | 30% | $30 Billion | 190,000 | $82 Million | 521 | Assumes lower efficiency gains and moderate health impact, using conservative QALY model. |
| Base Case | 50% | $50 Billion | 840,000 | $137 Million | 2,301 | The central estimate used in this analysis, based on the median QALY model. |
| Optimistic | 70% | $70 Billion | 3,650,000 | $192 Million | 10,000 | Assumes high efficiency and significant improvements in health outcomes, using optimistic QALY model. |
| Transformative (RECOVERY Trial-like) | 95% | $95 Billion | 3,650,000 | $260 Million | 10,000 | Reflects exceptional, RECOVERY-like efficiency and broad health benefits, using new optimistic QALY model. |
¶ Discussion of Uncertainty and Key Variables
While the figures are presented as daily point estimates for clarity, they represent the steady-state potential loss once the dFDA platform is fully adopted. The actual daily loss on any given day depends on several key variables that introduce uncertainty:
- Adoption Rate (): The calculations above implicitly assume full adoption (). As modeled in the NPV analysis in the ROI Analysis section, adoption will be gradual. Therefore, the daily opportunity cost will ramp up over time, starting smaller and growing as the platform's use becomes standard. The figures represent the daily cost once that potential is reached.
- Magnitude of R&D Savings (): The percentage reduction in R&D costs is a critical variable. While the 95% reduction seen in the RECOVERY trial demonstrates what is possible, the system-wide average may be lower. The sensitivity table addresses this by showing a range from 30% to 95%.
- Realization of QALY Gains: The link between a more efficient research ecosystem and concrete health outcomes (QALYs) is complex. The estimates for QALYs gained are based on evidence from studies on the value of faster drug access and improved prevention, but the exact magnitude of the dFDA's impact remains a projection.
Conclusion: Despite these uncertainties, the analysis consistently shows that the daily opportunity cost of inaction is substantial across all plausible scenarios. Every day that the current inefficient, slow, and expensive paradigm for clinical research is maintained, society forgoes hundreds of quality-adjusted life-years and tens to hundreds of millions of dollars in value. This provides a powerful, daily reminder of the urgency and immense potential of the dFDA initiative.
¶ Source Quotes for Key Parameters
-
$100 billion global annual clinical trial expenditure
"The global clinical trials market size was valued at USD 60.94 billion in 2024. The market is projected to grow from USD 64.94 billion in 2025 to USD 104.41 billion by 2032..."
— Fortune Business Insights, May 2024
"The global clinical trials market accounted for USD 59 billion in 2024. The market is anticipated to grow from USD 62.4 billion in 2025 to USD 98.9 billion in 2034..."
— Global Market Insights, Feb 2024 -
$500 per patient (RECOVERY trial)
"The cost per patient in the RECOVERY trial was approximately $500, compared to $40,000–$120,000+ per patient in traditional Phase III trials."
— RECOVERY Trial Wiki (citing Manhattan Institute and NCBI), ProRelix Research, Power -
$360B U.S. drug spend
"U.S. annual prescription drug spending is ~$360B."
— CMS National Health Expenditure Data
"The U.S. spent $360 billion on prescription drugs in 2019."
— Commonwealth Fund -
$3 saved per $1 prevention
"Every $1 spent on prevention saves ~$3."
— Trust for America's Health, 2013 -
$10M Value of Statistical Life (VSL)
"The value of a statistical life (VSL) is $10 million (2021 dollars)."
— U.S. Department of Transportation, 2021 Guidance -
$100,000–$150,000 per QALY
"ICER's health benefit price benchmark (HBPB) will continue to be reported using the standard range from $100,000 to $150,000 per QALY and per evLYG."
— ICER Reference Case
"The Institute for Clinical and Economic Review (ICER) often uses a benchmark range of $100,000 to $150,000 per QALY."
— ICER Value Assessment Framework -
840,000 QALYs gained/year
The dFDA platform is projected to generate 840,000 QALYs per year in its base case scenario. This is a composite metric derived from a detailed model in the appendix, which sums the impacts of (A) accelerating existing drug development, (B) improving preventative care with real-world evidence, and (C) enabling new therapies for previously untreatable rare diseases. The model is based on inputs from sources including the NBER, CDC, and GAO.
— See this document's Appendix Detailed QALY Calculation Model -
RECOVERY trial cost reduction
"The UK RECOVERY trial, a prime example of efficient trial design akin to dFDA principles, achieved cost reductions of ~80-98% per patient compared to traditional trials."
— RECOVERY Trial Wiki -
Prevention savings calculation
"If preventive spending increases by $205B and each $1 saves $3, additional savings = $205B × 3 = $615B/year."
— Trust for America's Health, 2013 -
U.S. prescription drug prices 50–90% higher than peer countries
"U.S. prescription drug prices are 50–90% higher than in peer countries."
— Commonwealth Fund, 2017 -
QALY definition and use
"The quality-adjusted life year (QALY) is the academic standard for measuring how well all different kinds of medical treatments lengthen and/or improve patients' lives, and therefore the metric has served as a fundamental component of cost-effectiveness analyses in the US and around the world for more than 30 years."
— ICER
¶ Final ROI and Net Benefit
- Central ROI Estimate: 463:1
- Central Net Benefit (10-Year, Discounted): ~$249 Billion
- Dominant Health Intervention: The dFDA is cost-saving while simultaneously generating substantial health gains (QALYs), making it a dominant intervention from a health economics perspective.
¶ Comparative Cost-Effectiveness: dFDA vs. Other Public Health Interventions
To provide context for the dFDA platform's impact, the chart below visualizes its cost-effectiveness against other well-understood public health programs. The metric used is Quality-Adjusted Life Years (QALYs) Gained per $1 Million of Spending. A higher number signifies greater cost-effectiveness.
For standard interventions, this value is calculated as $1,000,000 / ICER, where the ICER (Incremental Cost-Effectiveness Ratio) is the cost to gain one QALY. For dominant interventions that are both more effective and less expensive, the ICER is negative, and this metric isn't strictly applicable. For these cases, an illustrative range is used to represent their high value.
All data used in the chart is derived from the table and sources below.
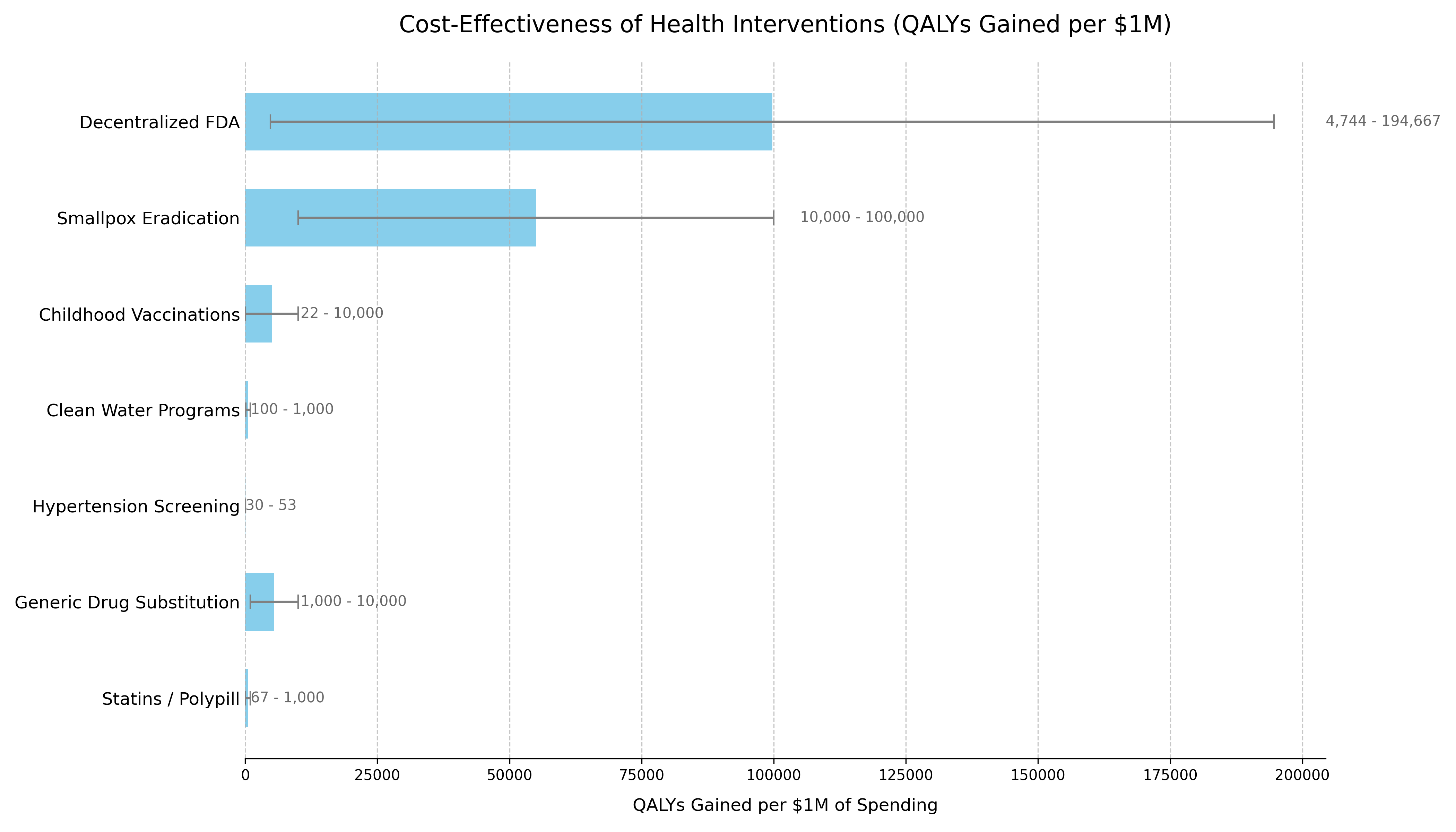
The following table provides the data and sources that support the chart. The list is ordered to match the chart's presentation.
| Intervention | QALYs Gained per $1M Spending¹ | Typical ICER Range (Cost per QALY Gained) | Classification | Source / Evidence |
|---|---|---|---|---|
| dFDA Platform | 4,744 - 194,667 | -$260,000 to -$19,000² | Dominant | This analysis's Sensitivity Analysis. Based on $18.75M-$40.05M annual costs generating 840,000-3.65M QALYs annually. |
| Smallpox Eradication | 10,000 - 100,000+³ | Dominant (Cost-Saving) | Dominant | The $300M program (1967-1980) prevents 5M annual deaths. Benefit-cost ratio exceeds 100:1. Standard ICER calculation is impractical due to its unprecedented scale. WHO, 2010) |
| Childhood Vaccinations | 22 - 10,000+³ | Often Dominant to ~$100,000 | Dominant / Highly Cost-Effective | CDC estimates routine childhood vaccinations prevent 32M hospitalizations and 1.1M deaths among 1994-2023 US birth cohorts, with $2.9T in societal cost savings. (CDC, 2023) |
| Clean Water Programs | 100 - 1,000 | ~$1,000 - $10,000 | Highly Cost-Effective | WHO estimates household water treatment costs $20-$500/DALY averted. Community water supply improvements cost $200-$2,000/DALY. (WHO, 2004) |
| Hypertension Screening | 30 - 50 | ~$20,000 - $33,000 | Highly Cost-Effective | Recent US studies show pharmacist-led hypertension management has ICERs under $50,000/QALY, with most interventions falling in the $20,000-$33,000 range. (JAMA Netw Open, 2023) |
| Generic Drug Substitution | 1,000 - 10,000+³ | Dominant (Cost-Saving) | Dominant | By definition cost-saving when therapeutic equivalence is maintained, with typical savings of 30-80% versus brand-name drugs. (WHO, 2015) |
| Statins / Polypill | 67 - 1,000+³ | Cost-Saving to ~$15,000 | Dominant / Highly Cost-Effective | Cost-saving in high-risk populations. ICERs range from dominant to $15k/QALY in lower-risk groups. (eClinicalMedicine, 2022) |
¶ Methodology Notes
- For interventions with positive ICERs:
1,000,000 / ICER - For the dFDA Platform:
(Annual QALYs Gained) / (Annual Cost in Millions) - Ranges reflect conservative to optimistic scenarios accounting for parameter uncertainties
² Negative ICER Interpretation:
- All dFDA scenarios show negative ICERs, indicating cost-saving while generating health benefits
- The platform is "dominant" - more effective and less costly than the status quo
- For cost-saving (dominant) interventions, standard QALY/$1M calculations are not applicable
- Values shown are illustrative to demonstrate relative cost-effectiveness
- Upper bounds represent the exceptional value of these interventions
¶ Data Limitations
- Historical interventions (e.g., smallpox) use retrospective analyses
- Direct comparisons between interventions should consider contextual differences
- All costs are in 2023 USD, adjusted using appropriate health inflation indices
- QALY calculations use standard health state utility weights where available
Conclusion: The dFDA initiative is not just a financially sound investment with a high ROI; it is one of the most impactful public health interventions conceivable. Its "dominant" cost-effectiveness profile is comparable to gold-standard programs like childhood vaccination and smoking cessation, but its scale of economic and health benefits is potentially orders of magnitude larger.
¶ Comparison to Other Major Public Investments
To provide context for the dFDA's estimated costs, it is useful to compare them to other significant U.S. government investments in health and technology. The dFDA's projected "Lean Ecosystem" cost of approximately $40 million per year (covering core platform operations plus medium-scope broader initiatives) is modest in comparison to other major federal projects.
| Initiative / Project | Approximate Cost / Budget (Annualized) | Comparison to dFDA Annual Cost | Source / Note |
|---|---|---|---|
| dFDA Platform (Lean Ecosystem) | ~$40 Million / year | 1x (Baseline) | This analysis |
| Cancer Moonshot Initiative | ~$257 Million / year ($1.8B over 7 years) | ~6.4x | 21st Century Cures Act |
| NIH "All of Us" Research Program | **~$500 Million / year (FY23 Approx. Budget) | ~12.5x | NIH Budget |
| HealthCare.gov (Initial Build) | ~$1.7 - $2.1 Billion (Total Upfront Cost) | ~42x - 52x (of one year's dFDA cost) | GAO Reports / Public Reporting |
| National Cancer Institute (NCI) | ~$7.2 Billion / year (FY25 Budget) | ~180x | NCI Budget Data |
Key Takeaway: The estimated annual cost of the dFDA initiative is an order of magnitude smaller than the budgets for other major national health priorities like the "All of Us" program or the Cancer Moonshot. It represents approximately 0.55% of the NCI's annual budget (calculated from dFDA annual cost and NCI budget). This comparison underscores that the dFDA platform is not only a high-leverage investment (due to its massive ROI) but also a remarkably cost-effective one relative to the scale of federal health and technology spending.
¶ Appendix: Detailed QALY Calculation Model
This appendix provides a transparent, component-based model for the aggregate QALY figures used in this analysis. The total QALY gain is the sum of three distinct benefit streams. For each stream, we define parameters for a Conservative, Base, and Optimistic scenario, with sources and rationale provided for each parameter.
¶ A. QALYs from Faster Drug Access
This stream models the benefit of accelerating the approval of new drugs that would likely be developed under the current paradigm, but more slowly.
-
Parameters:
- : Number of new drugs approved annually whose development is accelerated.
- Rationale: The FDA approves a significant number of new drugs each year, and the dFDA platform is expected to accelerate the development of a meaningful fraction of these.
- Source: The FDA consistently approves a substantial number of novel therapies. For example, in 2023, the Center for Drug Evaluation and Research (CDER) approved 55 novel drugs.
- Quote: "[In 2023], the Center for Drug Evaluation and Research (CDER) approved 55 novel drugs, either as new molecular entities (NMEs) under New Drug Applications (NDAs) or as new therapeutic biologics under Biologics License Applications (BLAs)." — Friends of Cancer Research
- : Average years of acceleration per drug.
- Rationale: The dFDA model, inspired by hyper-efficient trials like the RECOVERY trial, can drastically cut development timelines from years to months.
- Source: The RECOVERY trial demonstrated unprecedented speed in generating clinical results.
- Quote: "Days to First Major Result: <100" — The Conversation, via dFDA Wiki
- : Average QALYs gained per drug, per year of earlier access.
- Rationale: Accelerating access to effective drugs has a direct and significant impact on life-years and quality of life.
- : Number of new drugs approved annually whose development is accelerated.
-
Formula:
-
Scenario Values:
- Conservative: 15 drugs/year 1 year acceleration 6,000 QALYs/drug = 90,000 QALYs
- Base: 20 drugs/year 1.5 years acceleration 8,000 QALYs/drug = 240,000 QALYs
- Optimistic: 25 drugs/year 2 years acceleration 10,000 QALYs/drug = 500,000 QALYs
¶ B. QALYs from Improved Prevention and Real-World Evidence (RWE)
This stream models the benefit of using the dFDA's vast data to optimize preventative care and the use of existing treatments.
-
Parameters:
- : Number of patients benefiting from new preventative guidelines or RWE-driven treatment changes.
- Rationale: Chronic diseases affect a vast portion of the population, and even small improvements in prevention or treatment optimization, scaled across millions of people, can generate substantial health gains.
- Source: The CDC notes the immense scale of chronic disease in the United States.
- Quote: "Six in ten adults in the US have a chronic disease." — CDC, About Chronic Diseases
- : Average small QALY gain per impacted patient from better-targeted prevention or treatment.
- Rationale: While the per-person gain from preventative measures may be small in a single year, they are well-established. The value comes from applying these small gains to a very large population.
- Source: Health economic literature provides many examples of modest but important QALY gains from preventative care.
- Quote: "Statin treatment provides a gain of 0.20 QALYs in men aged 60 years." — BMJ, via NCBI
- : Number of patients benefiting from new preventative guidelines or RWE-driven treatment changes.
-
Formula:
-
Scenario Values:
- Conservative: 5 million patients 0.01 QALYs/patient = 50,000 QALYs
- Base: 10 million patients 0.01 QALYs/patient = 100,000 QALYs
- Optimistic: 15 million patients 0.01 QALYs/patient = 150,000 QALYs
¶ C. QALYs from Expanded Scope (New Therapies)
This stream models the benefit of enabling trials for therapies that are currently neglected due to high cost (e.g., rare diseases, unpatentable treatments, novel nutraceuticals). The model is based on the number of new therapies, the average patient population per therapy, and the QALY gain per patient.
-
Parameters:
- : Number of entirely new, effective therapies enabled per year for untreated conditions.
- Rationale: There is a vast unmet need in the rare disease space, with an estimated 7,000 to 10,000 known rare diseases and treatments for only about 5%. Lowering trial costs via the dFDA platform would catalyze R&D for this underserved population.
- Source: U.S. Government Accountability Office (GAO).
- Quote: "But only about 5% of the nearly 10,000 identified rare diseases have Food and Drug Administration-approved treatments." — GAO, Nov 2024
- : Average number of patients benefiting from a new rare disease therapy.
- Rationale: While "rare" in the US means affecting fewer than 200,000 people, the median prevalence is much lower. This estimate uses a conservative figure for the addressable population for a new, breakthrough therapy.
- Source: Analysis of Orphanet data suggests a median prevalence of 1-5 per 100,000 people. (Orphanet Journal of Rare Diseases)
- : Average QALY gain per patient receiving a transformative therapy.
- Rationale: A new therapy for a previously untreatable, life-threatening condition can have a profound impact, corresponding to many years of high-quality life.
- Source: Therapies for diseases like spinal muscular atrophy or certain inherited retinal diseases can be considered near-curative, generating dozens of QALYs per patient over a lifetime.
- : Number of entirely new, effective therapies enabled per year for untreated conditions.
-
Formula:
-
Scenario Values:
- Conservative: 5 new therapies/year 2,000 patients/therapy 5 QALYs/patient = 50,000 QALYs
- Base: 10 new therapies/year 5,000 patients/therapy 10 QALYs/patient = 500,000 QALYs
- Optimistic: 20 new therapies/year 10,000 patients/therapy 15 QALYs/patient = 3,000,000 QALYs
¶ Summary of Total Annual QALY Gains
This table summarizes the component calculations and derives the total QALY range used in the main analysis. The final totals are hyperlinked back to the main body of the analysis. The model demonstrates that even with conservative, evidence-based inputs, the potential health benefit is substantial, providing a strong rationale for the dFDA initiative.
| QALY Benefit Stream | Conservative Scenario | Base Scenario | Optimistic Scenario |
|---|---|---|---|
| A. Faster Drug Access | 90,000 | 240,000 | 500,000 |
| B. Improved Prevention/RWE | 50,000 | 100,000 | 150,000 |
| C. Expanded Scope | 50,000 | 500,000 | 3,000,000 |
| Total Annual QALYs | 190,000 | 840,000 | 3,650,000 |
¶ Sources
- "The quality-adjusted life year (QALY) is the academic standard for measuring how well all different kinds of medical treatments lengthen and/or improve patients' lives, and therefore the metric has served as a fundamental component of cost-effectiveness analyses in the US and around the world for more than 30 years." (ICER)
- "ICER's health benefit price benchmark (HBPB) will continue to be reported using the standard range from $100,000 to $150,000 per QALY and per evLYG." (ICER Reference Case)
- "Each year of delayed access to curative therapy for hepatitis C costs 0.2–1.1 QALYs per patient." (Pho et al., 2015)
- "Syphilis causes substantial health losses in adults and children... The average number of discounted lifetime QALYs lost per infection as 0.09." (Lee et al., 2022)
- "Statin treatment provides a gain of 0.20 QALYs in men aged 60 years." (BMJ)